After years of decreasing, the rates of cervical cancer in Canada have stabilized, as reported by the Canadian Cancer Society. This concerning development is worrisome to experts, especially considering that cervical cancer is a preventable form of cancer. Between 1984 and 2005, there was a consistent decline in cervical cancer rates. However, a recent report from the Canadian Cancer Statistics Advisory Committee indicates a plateau in the annual percentage change for cervical cancer rates from 2005 to 2021, hovering just below zero.
Although cervical cancer is not among the leading causes of cancer-related deaths for females in Canada, the report highlights that each of the projected 430 deaths in 2025 due to this cancer could have been prevented. Cervical cancer is largely preventable through the vaccination against and screening for human papillomavirus (HPV), a sexually transmitted infection known to cause cervical cancer and certain head and neck cancers.
The World Health Organization aims to virtually eradicate cervical cancer globally by reducing the incidence to fewer than four cases per 100,000 females, while Canada has set a target to eliminate it within the country by 2040. However, with the current trend, it seems unlikely that this goal will be achieved on time, according to Brandon Purcell, the advocacy manager of prevention and early detection at the Canadian Cancer Society.
The report highlights a troubling plateau in cervical cancer rates attributed to lower HPV vaccination rates, decreased screening rates, and gaps in follow-up care. This news is disheartening to Shannon Pethick, a cervical cancer survivor, who emphasizes the importance of regular screenings and prevention methods, stressing the minimal inconvenience of screenings compared to the potential consequences of neglecting them.
To combat the stagnation in progress towards eliminating cervical cancer, experts suggest implementing policies to enhance vaccination coverage, increase screening accessibility, and transition to HPV testing over pap testing. Dr. Amanda Selk, an obstetrician gynecologist, underscores the need for innovative approaches to screening, especially considering the impact of the COVID-19 pandemic on healthcare access.
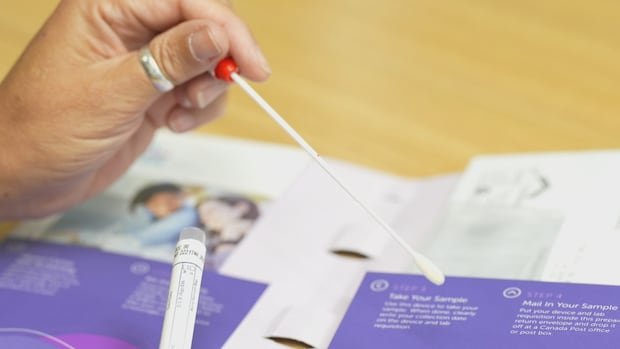
Introducing at-home testing, already successful in some regions, could revolutionize screening strategies. The transition from pap testing to HPV testing is also recommended, as it provides a more proactive approach by identifying potential cancer development. The effectiveness of the HPV vaccine in preventing cervical cancer is well-documented, with studies showing zero cases of cervical cancer among fully vaccinated individuals.
Efforts to expand vaccination coverage, including unconventional campaigns like those seen in Sweden, have proven effective in increasing HPV vaccination rates. Additionally, initiatives to provide catch-up vaccines for those who missed out during their school years could further enhance protection against HPV-related cancers.
Aside from the concerning plateau in cervical cancer rates, the overall cancer landscape in Canada shows positive trends, with increased survival rates and reduced incidence of lung and colorectal cancers in recent years. These findings underscore the importance of continued vigilance in cancer prevention and control efforts across the country.